Our resident GP explains newborn jaundice, detailing what all new parents need to know about identifying, testing for and managing this medical condition.
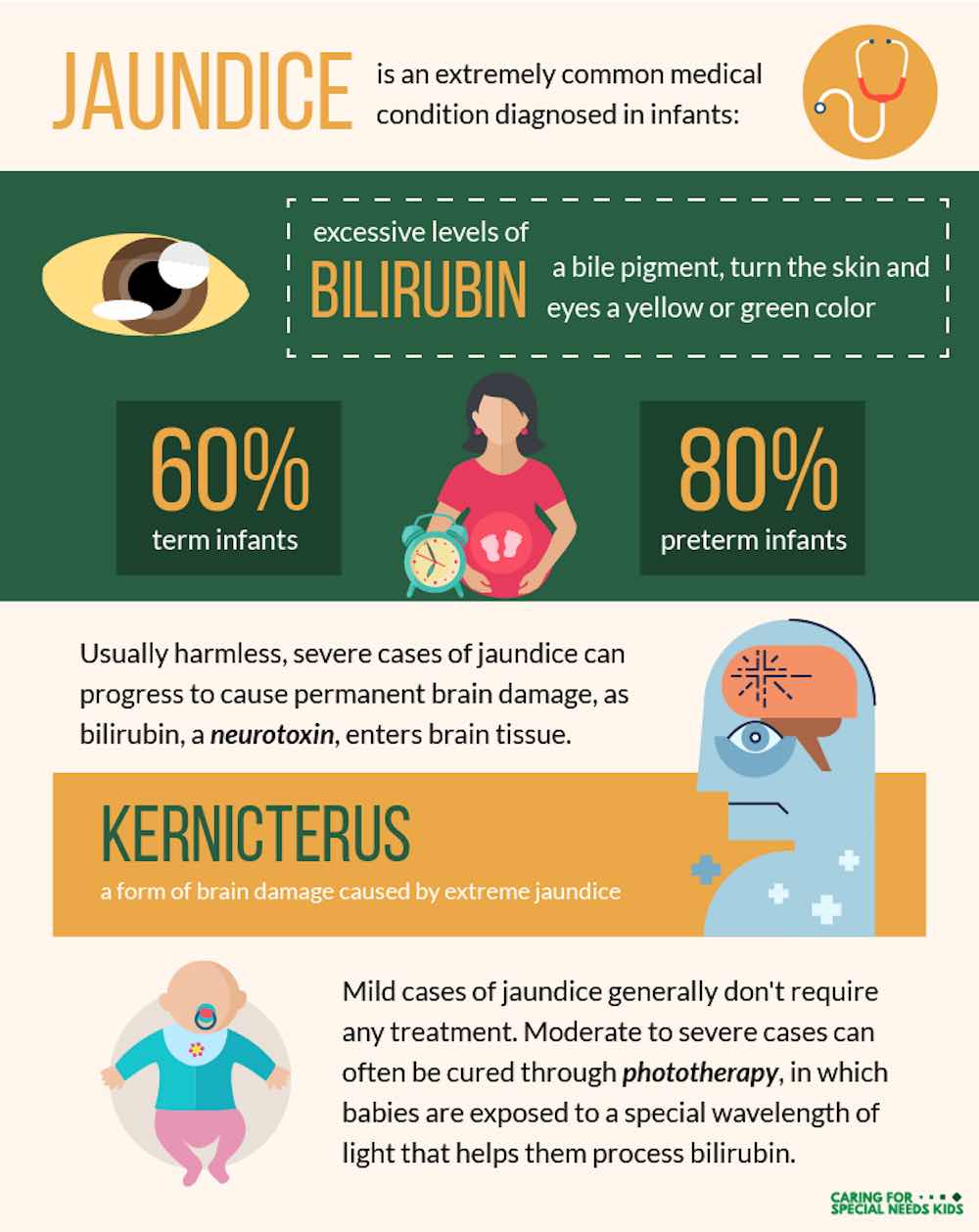
Jaundice is a very common occurrence in newborn babies, with over half affected to some degree (more if premature). It is usually noticed a few days after birth as the yellowish colouring of the baby’s skin and the whites of their eyes. They often look like they have quite a nice tan! It usually settles within a couple of weeks.
Most of the time newborn jaundice is harmless
Most of the time jaundice is harmless and does not indicate any underlying problems. However, it can be either a sign of underlying disease OR even if the cause itself is not serious, jaundice may require a simple treatment to prevent long-term harm to your baby.
So what is newborn jaundice?
Jaundice is caused by the breakdown of red blood cells (the cells that carry oxygen around the body). When red blood cells break down they release something called bilirubin. Normally this is processed by the liver and then removed from the body via the urine/stool. Early on, the baby’s liver is not fully functioning so it is often a bit overwhelmed and unable to process this properly. This causes bilirubin to accumulate and produce the characteristic yellow discoloration.
What causes newborn jaundice?
There is a range of causes. Most of the time, newborn jaundice is harmless and related to the liver’s immaturity with no long-term consequence. However, there are some more serious causes that may need to be monitored or treated urgently.
- Normal “physiological” jaundice (usually resolves in 2 weeks)
- More common with delayed cord clamping which is a relatively common practice now to ensure the baby receives more red blood cells from its mother (and hence more iron). The trade off is more red blood cells, which equals more breakdown products (bilirubin) – so baby may become more jaundiced.
- More common with birth trauma – for example, if your baby has a big bruise on its head (cephalohaematoma), which is often seen with assisted deliveries, the blood in the bruising breaks down and again may cause higher levels of bilirubin
- More common in premature babies with less mature livers
- Breast milk jaundice – some babies who are breastfed can appear jaundiced for prolonged periods. As long as other causes are ruled out this is of no concern and ongoing breastfeeding is absolutely fine (in fact encouraged). My new bub is currently sporting a lovely breast milk jaundice “glow”!
- Some infections, thyroid problems, metabolic problems
- Blood type incompatibility – this is when the mum and baby’s blood types are different and antibodies from the mum attack the baby’s red cells causing more of them to breakdown
- Biliary atresia – this is rare and is caused by a problem in the tubing of the bile ducts in the liver. This is a serious cause that needs to be diagnosed and treated ASAP. These babies will have very pale (almost white) stools and dark urine – see your doctor ASAP if you notice this.
When could jaundice be a concern? Signs to look for that could mean newborn jaundice
- If you think baby is yellow within the first 48 hours of life mention it to your midwife/doctor
- Baby’s poo is very pale or the urine very dark
- Your baby is not feeding well, seems very lethargic
- Visually jaundice is still noticeable after two weeks
- If newborn jaundice seems to be getting more noticeable after a week
What tests are required?
It is common that no testing is required. Often doctors will look at how jaundiced your baby is (it tends to start at the head and work its way down the body), consider their age and other symptoms and then decide if any tests are necessary.
If we are worried about the degree of jaundice, the first step is a blood test to check the bilirubin level (often done as a heel prick test). This is interpreted along with your baby’s age/size to determine if they need help excreting the extra bilirubin (in the form of UV light therapy). If we are worried about other causes like infection, thyroid problems, blood group mismatch or structural problems around the liver or bile system other tests will be done (usually starting with blood tests and possibly imaging tests like ultrasound depending on what the concern is).
Treatment of newborn jaundice
It is common that no treatment is required. Doctors use a reference of safe levels of bilirubin (which vary according to age and weight) and under these levels babies just need monitoring. If the levels are too high (the danger here being damage to part of the brain – “kernicterus”) then phototherapy is used. This uses UV lights to help the body break down extra bilirubin. Your baby is placed under a blanket or in a cot with UV lamp for a day or so. Its eyes will be covered to protect them.
This treatment has minimal side effects; the main issue is they may need extra feeds to prevent dehydration during this time. In some cases, very severe jaundice may require something called an exchange transfusion – this is a bit like a blood transfusion but is very rarely required. The baby’s blood test will usually be monitored every 12-24hours if treatment is required to determine how long to continue. Often only a day or two is required.
Prevention of jaundice in newborns
In most cases, jaundice is not preventable. Keeping well hydrated helps. The only type that is preventable is the blood group incompatibility types. Because of this mothers with a negative blood group are given injections of Anti-D during their pregnancies. The aim of this is to prevent the mother producing the antibodies against her baby’s blood. These can later attack the red blood cells.
Want to know more about newborn jaundice – here’s some resources to explore:
- Medical News Today: Jaundice
- Sydney Children’s Health Network: Jaundice Fact Sheet
- Perth Children’s Hospital Guide to Newborn Jaundice